NURSING 3PF1 Study Guide - Summer 2018, Comprehensive Midterm Notes - Syndrome, Muscle, Ischemia

NURSING 3PF1
MIDTERM EXAM
STUDY GUIDE
Fall 2018

1
Alterations in Reproductive Functions
- HPO axis: hypothalamic pituitary ovarian axis; the main hormonal feedback pathway responsible for the reproductive system
- Menarche: the first menstrual cycle achieved
- Os: the opening from the uterus through the cervix into the vagina; can measure the dilatation to monitor the progress of labour
- Fundus: the top of the uterus; during pregnancy this can be used as one measurement point for monitoring growth of the fetus (symphysis-fundal
height); after delivery the fundus is palpated to monitor the resolution phase
- Infertility: failure to achieve pregnancy after one year of unprotected intercourse; if the female patient is over 35 years then the interval is shortened
to 6 months
- IUI: intra uterine insemination, where a small catheter is passed into the uterus via the vagina and cervix so that the semen may be instilled directly
into the uterus
- IVF: in vitro fertilization; the process by which the ova and semen are collected from the individuals and mixed together to permit fertilization to
occur; after 3-5 days, 1-2 growing embryos are returned to the uterus, any remaining fertilized ova can be frozen for future attempts
- Prenatal (antenatal): the period of time from conception to the birth of the infant
- Postnatal: the period of time from the delivery of the infant until complete resolution of the body to the pre-pregnant state, usually 6-8 weeks
- Parity: the number of deliveries that a woman has had over 20 weeks gestation, when this number is over 5 this is considered to be a state of grand
multiparity, or the woman is referred to as a grand multipara
GTPAL = a short hand for describing a woman’s obstetrical history
- G: gravida, or total number of pregnancies, including miscarriages, abortions and stillbirths
- T: term; the total number of deliveries over 37 weeks gestational age
- P: preterm; the total number of deliveries between 20 and 37 weeks gestational age
- A: abortions; spontaneous (occurring on their own) or therapeutic (occurring by surgical intervention)
- L: the number of living children
Viability: the point at which should a fetus deliver there is a reasonable expectation of survival, usually defined as 500gm or more than 20 weeks
gestation. This is a contentious issue and will not be further discussed
Fetal Presentation:
- Macrosomia: when the fetal head size has grown larger than can be passed vaginally
- Polyhydramnios: the amount of amniotic fluid is more than 2 standard deviations above the norm for gestational age
Normal Female Anatomy
➢ The sexual differentiation of an embryo occurs around the 7th week of gestation and is determined by the sex chromosome: XX = female or XY =
male
• The Y chromosome (or SYR protein) is the testes determining factor
• Without this protein, the vagina, uterus and fallopian tubes will develop (otherwise known as Mullerian ducts)
➢ The ovaries produce the secondary oocytes and hormones such as estrogen, progesterone, inhibin and relaxin. At birth, the ovaries of the female
newborn contain all their primary oocytes and their secondary oocytes are formed after puberty once a month at ovulation
➢ The uterine tubes or fallopian tubes transport the secondary oocyte to the uterus and normally these tubes are the sites where fertilization occurs
➢ The uterus is the site of implantation for the fertilized ovum. This muscular organ is where the fetus will develop during pregnancy and will promote
the progression of labour. Three layers of the uterus are the endometrium, myometrium and perimetrium
➢ The vagina is the receptacle for sperm during intercourse and also the passageway for childbirth
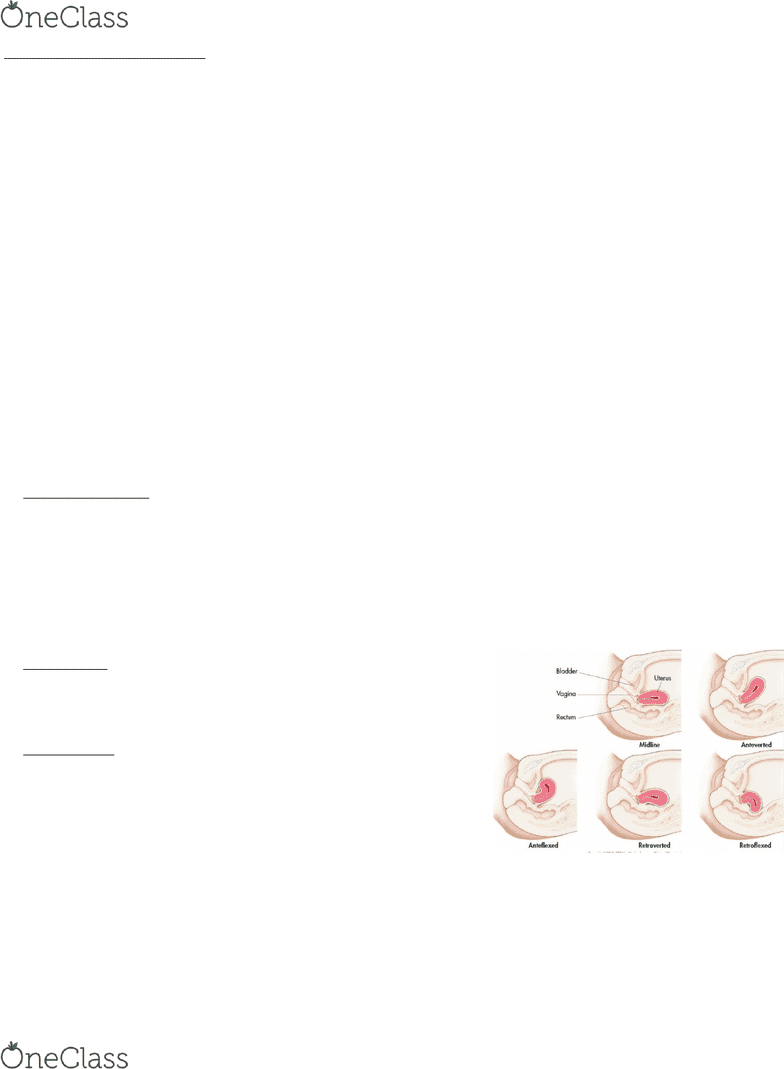
Uterine Position:
The position of the uterus in the pelvis is something females are born with and this uterine
position it will remain the same throughout their lifetime. During a routine pelvic
examination, a clinician can palpate the uterus during a bimanual examination to determine
their uterine lie or position as per the diagram. This does not affect fertility.
Female Hormones
➢ Onset of puberty the hypothalamic neurosecretory cells release gonadotropin releasing
hormone (GnRH) which subsequently binds to the anterior pituitary cells called the
gonadotrops and stimulates them to increase the secretion of the follicular stimulating
hormone (FSH) and luteinizing hormone (LH)
o FSH stimulates the growth of follicles of the ovaries to produce
estrogen, progesterone and inhibin
o LH is responsible for stimulating the ovulation (LH surge) and the
formation of the corpus luteum
- Estrogen:
• development and maintenance of the female reproductive structures
• secondary female characteristics such as adipose tissue deposition, voice pitch, broad pelvis and pattern of hair growth
• estrogen can work synergistically with GH to increase protein synthesis including bones
• lowers blood cholesterol
• moderate levels inhibit release of GnRH, FSH and LH
- Progesterone:
• secreted mainly by the cells of the corpus luteum in the last two week of the menstrual cycle
• works with estrogen to prepare and maintain the endometrium and to prepare the mammary glands for lactation
• inhibits release of GnRH and LH
find more resources at oneclass.com
find more resources at oneclass.com

2
- Relaxin:
• produced by the corpus luteum
• inhibits contractions of uterine smooth muscle
• during labor, increases flexibility of pubic
symphysis and dilates uterine cervix
- Inhibin:
• secreted by the granulosa cells of the follicles
and together with the levels of estrogen and
progesterone, these hormones provide feedback
for the HPO axis, either stimulating or
inhibiting further release of FSH and LH
Female Monthly Cycle
Normal: 24-36 days with the biggest variation occurring
during the pre-ovulatory phase
Day 1-5
• The menstrual phase when the uterus sheds all but the deepest layers of the endometrium (approx. 50-150ml of blood, tissue, fluid, mucus
and epithelial cells)
• This discharge is due to the decreased amount of progesterone and estrogen
o we can manipulate these hormones using oral contraceptives; when the woman stops taking the active hormones, the level of
progesterone particularly decreases and this withdrawal promotes the bleeding
• At this point the ovarian hormones are at the lowest levels and this stimulates the secretion of GnRH and subsequently FSH and LH
Day 6-14
• The variable pre-ovulatory phase and under the influence of FSH the maturation of the dominant follicle occurs.
• This phase is the proliferative phase of the uterus as estrogen promotes the endometrial growth
Day 14
• Ovulation occurs when the secondary oocyte is released into the pelvic cavity, surrounded by the zone pelucida and corona radiata
• The leftover cells in the ovary become the corpus luteum under the influence of LH and this structure then secretes estrogen, progesterone,
inhibin and relaxin
Day 15-28
• Post-ovulatory phase
• Progesterone and estrogen secreted by the corpus luteum causes further growth and coiling of the endometrial glands and thickening of the
endometrium, all in preparation for a fertilized ovum
• Without a fertilized ovum, the corpus luteum degenerates, leading to a decreased amount of progesterone
• With the withdrawal of progesterone, menstruation occurs
Implantation
- Zygote: fertilized ovum
- Blastocyst: collection of rapidly proliferating cells; up to 2 weeks
- Embryo: 2-8 weeks
- Fetus: 8 weeks to birth
- To achieve pregnancy the fertilized zygote must be able to
penetrate into the endometrial layer of the uterus; takes several
days
- Day 10-12 post-fertilization begin to see a rise in the β subunit
of human chorionic gonadotrope hormone or hCG (the marker
used to detect pregnancy in both urine and blood)
- Within a few hours after implantation, the trophoblast
(specialized cells around the blastocyst) will begin to produce
hCG – specifically produced during pregnancy to maintain the
corpus luteum, which produces the increasing amounts of
progesterone needed to support and thicken the uterine lining
- If hCG levels are insufficient, the corpus luteum will regress,
progesterone levels will drop and the sloughing of the
endometrial layer will occur
- Typically, the β-hCG value will double every two days in early
pregnancy and clinically this fact is used to support viability of
the pregnancy or to rule out ectopic pregnancy
find more resources at oneclass.com
find more resources at oneclass.com
Document Summary
Hpo axis: hypothalamic pituitary ovarian axis; the main hormonal feedback pathway responsible for the reproductive system. Os: the opening from the uterus through the cervix into the vagina; can measure the dilatation to monitor the progress of labour. Fundus: the top of the uterus; during pregnancy this can be used as one measurement point for monitoring growth of the fetus (symphysis-fundal height); after delivery the fundus is palpated to monitor the resolution phase. Infertility: failure to achieve pregnancy after one year of unprotected intercourse; if the female patient is over 35 years then the interval is shortened to 6 months. Iui: intra uterine insemination, where a small catheter is passed into the uterus via the vagina and cervix so that the semen may be instilled directly into the uterus. Prenatal (antenatal): the period of time from conception to the birth of the infant.
